Predicting Future Health Care Needs with Data-Driven Segmentation
In today’s world, healthcare systems are facing increasing pressure due to aging populations and a rising prevalence of chronic conditions. These trends demand innovative solutions to ensure efficient and effective patient care. One promising approach involves using data-driven population segmentation to predict healthcare needs and tailor interventions accordingly.
First, though, I have to editorialize. I don’t like the phrase data-driven. I’ve tried to purge it from my vocabulary. The reason is that data-driven implies a mechanistic approach to decision-making when in reality, there is a much more complex sense-making approach that must take place when considering the results of any survey, metric, or interview. I much, much, MUCH prefer to use the term “data-informed” in my work. But since this wasn’t my study and not my article, I’ll defer to the author’s terminology.
(•̀⤙•́ )
A recent study explored this by analyzing health data from over 400,000 patients in Wales. This study used advanced techniques to create segments of the population based on their healthcare usage and chronic conditions. The aim was to see if these segments could predict future healthcare events like emergency admissions, GP visits, and even mortality.
Why Segmentation Matters
Population segmentation is like dividing a classroom into study groups based on students’ strengths and needs. In healthcare, this means grouping people based on their health characteristics and how they use medical services. By doing so, healthcare providers can better understand the needs of different groups and design targeted interventions.
This study focused on a data-driven approach using k-means clustering (it’s a pretty basic technique). This technique grouped patients based on their use of healthcare services (like GP visits and hospital admissions) and the number of chronic conditions they had.
The Study’s Method and Findings
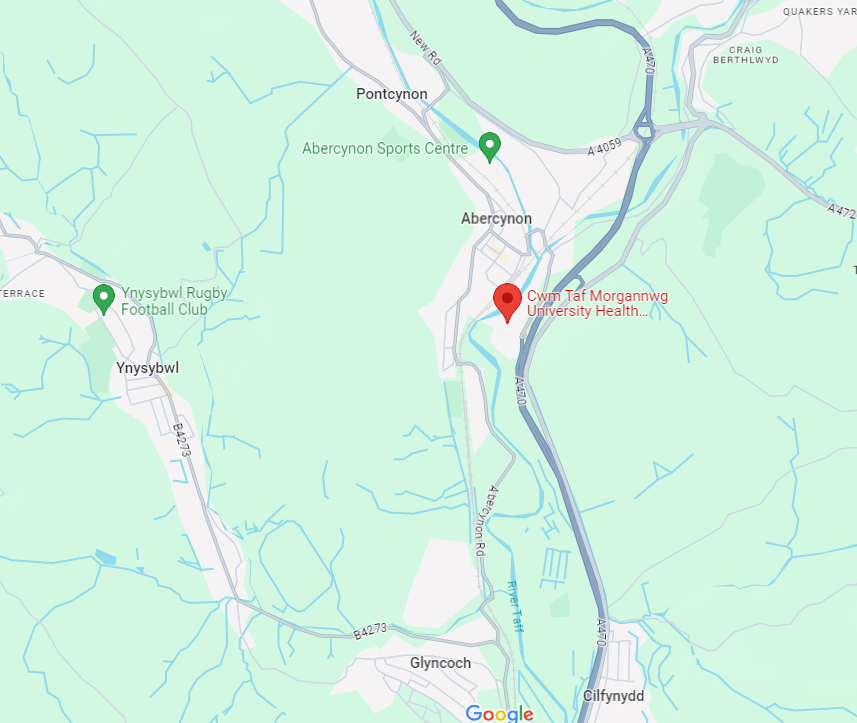
The research was conducted in the Cwm Taf Morgannwg University Health Board area in Wales, using data from 412,997 patients. The data included records of GP visits, hospital admissions, prescriptions, and more. Based on these factors, the researchers created ten distinct segments of the population.
The key findings of the study were:
- Improved Prediction with Segments: Adding these segments to traditional demographic models (age, sex, deprivation) improved the ability to predict future healthcare events significantly. For instance, the prediction accuracy for emergency admissions increased from an AUC (a measure of prediction accuracy) of 0.65 to 0.73.
- Effective Alone: The segments alone were nearly as predictive as the full models that included demographic information, indicating their robustness.
- Importance of Chronic Conditions: Including data on chronic conditions was crucial, particularly for predicting mortality.
Why This Matters for Public Health
For public health practitioners, these findings are significant. Predicting who is at risk of needing intensive healthcare allows for proactive measures. Instead of waiting for emergencies, healthcare providers can offer preventative care and support to those most likely to need it. This can reduce emergency admissions and improve overall health outcomes.
For example, suppose a segment of the population is identified as high risk for frequent hospital visits. In that case, healthcare providers can develop targeted interventions, such as home visits, chronic disease management programs, and more frequent check-ups. This not only improves patient outcomes but also alleviates the burden on emergency services.
Practical Applications
- Targeted Interventions: Healthcare providers can use segmentation to identify high-risk groups and tailor interventions to their specific needs.
- Resource Allocation: By understanding which segments are likely to require more intensive care, healthcare systems can allocate resources more effectively, ensuring that high-need groups get the attention they require.
- Policy Making: Policymakers can use these insights to develop strategies that focus on prevention and early intervention, ultimately aiming to reduce the strain on healthcare systems.
A Real-World Example
Imagine a local health board discovers through segmentation that a particular group of elderly patients with multiple chronic conditions is at high risk for emergency hospital admissions. Armed with this information, the board can implement a targeted intervention program. This might include regular home visits from healthcare professionals, personalized care plans, and support services for managing chronic conditions at home. By addressing these needs proactively, the health board can reduce emergency admissions and improve the quality of life for these patients.
Let us know in the comments!
- Have you or someone you know experienced a health intervention that felt tailored to your specific needs? How did it impact your healthcare experience?
- What do you think are the most significant barriers to implementing data-driven healthcare solutions in your community?
SEO Focus Key Phrase
Be a Health Innovator – Get Weekly Updates!
Stay informed and active. Subscribe for free and share this blog to make a difference in public health.
About the Author
Dr. Jonathan P. Scaccia, PhD, is a clinical-community psychologist with expertise in public health science and practice. He has led evaluation and research initiatives focusing on health equity, vaccine distribution, and organizational readiness. Dr. Scaccia has contributed to federal suicide prevention programs and vaccine equity strategies. He has been recognized for his impactful work and is a leading voice in advancing public health practices.