Yes, Politics Shapes Cancer Outcomes
A few months ago, before things took a nosedive, we spoke to Nancy Kriegar about her work looking at the intersection of health and political belief systems. You can revisit below.
Now, Dr. Kriegar has a new article looking at how politics shape cancer outcomes.
Let’s start with a basic principle. Many cancer deaths are preventable.
Modeling suggests up to 79% of colorectal, 25% of breast, and 100% of cervical cancer deaths could be averted with screening. Yet who holds power in a state is linked to when cancers are found and who dies too soon.
1) Power matters: conservative control → worse outcomes
States with more conservative political metrics, like Republican trifectas, lower scores on a state policy index, or more conservative voting records in Congress, tend to have more late-stage diagnoses (breast and colorectal) and higher premature cancer mortality. This pattern holds even when looking across different ways of measuring politics (ideology of elected officials, electoral outcomes, policy bundles).
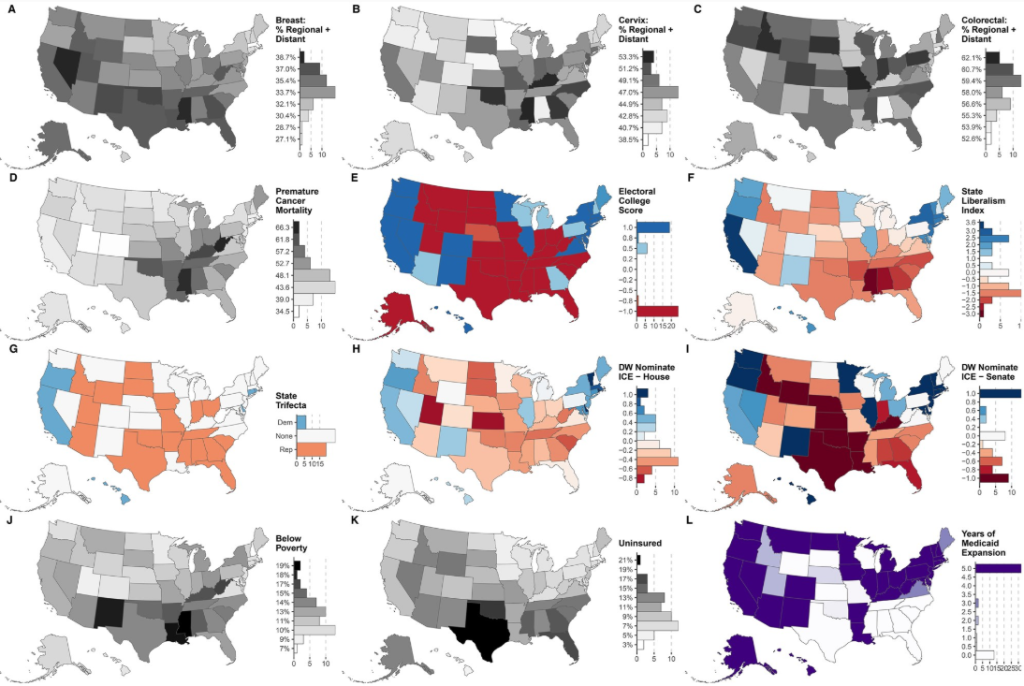
From the article, “Maps of state-level data for study cancer outcomes, political metrics, and covariates: (1) outcomes: age-standardized cancer stage at diagnosis (breast [female], cervix, colorectal) for adults at or above age at which screening is first recommended (% regional + distant) and cancer premature mortality rate (death before age 65) (panels A-D), (2) political metrics (panels E-I), and (3) covariates (panels J-L), for 50 US states and the District of Columbia (2017-2021).”
2) Insurance and poverty explain a lot—but not all
Yes, poverty, uninsurance, and Medicaid expansion status are big drivers of cancer stage and early death. Adjusting for these factors reduces many political–health links. But the study still finds independent associations for several political metrics, especially elected officials’ voting ideology and broad policy bundles, suggesting that political choices shape the conditions that shape health.
3) Screening access is the fast lever
Cancer stage at diagnosis moves quickly when access changes. Policies that expand coverage, reduce out-of-pocket costs, and bring services closer to people (mobile mammography, weekend colonoscopy preps, HPV testing with follow-up) can shift diagnoses toward earlier stages, the difference between treatable and tragic. Transportation, paid time off, and language access also matter.
Why it matters: This shows that policy environments either remove barriers to care or build them. The study’s bottom line: broader political choices, namely, who governs, what gets funded, and which protections exist, are tied to real cancer outcomes in every community.
What leaders can do now:
- Expand and simplify access (Medicaid, marketplace outreach, safety-net funding).
- Invest in practical supports (transport, childcare, paid time off).
- Track stage-at-diagnosis and premature mortality as equity metrics and align policy to move them.
Policies are prevention tools. When power shifts, screening, stage, and survival can shift too.