What Happens When Hospitals Come to Your Home?
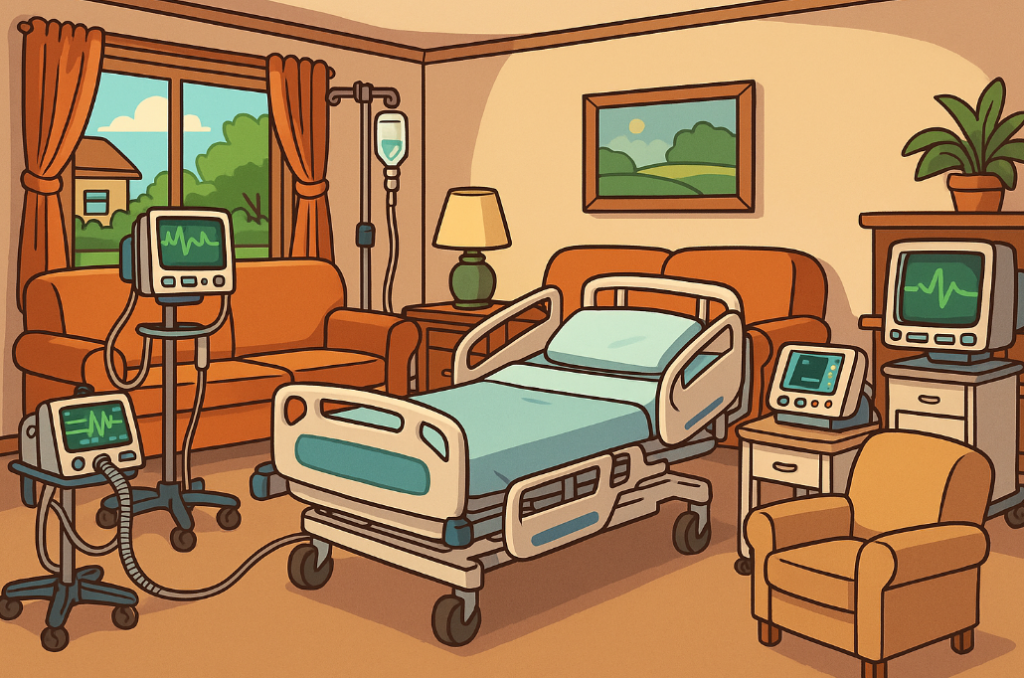
That’s the dream, right? No sterile fluorescent lights. No noisy hallways. Just healing in the comfort of your own bed.
That’s the promise of Hospital at Home (HaH), also known in the UK as virtual wards. It’s a growing model where patients get hospital-level care, like IV meds, vitals monitoring, and daily check-ins, right from their living rooms. The concept has exploded post-COVID, especially in England, where the NHS hopes to treat 50,000 patients a month this way.
But a new study from researchers in the UK asks a critical question: What happens when something goes wrong?
Virtual Wards: The Good, the Bad, and the Overlooked
To understand this new care frontier, the researchers didn’t just review documents or policies. They interviewed 12 experts—doctors, pharmacists, nurse practitioners—and held a focus group to test and refine their insights. Then, they did something novel: they built two models.
- A Logic Model mapping the ideal outcomes: better care, faster recovery, less pressure on hospitals.
- A Dark Logic Model exposing what could go wrong: miscommunication, fragmented records, digital exclusion, and even rising inequalities.
These visual maps aren’t just diagrams—they’re roadmaps for safer, smarter healthcare.
“Buy-In” Isn’t Just Bureaucracy—It’s Life or Death
One thing became clear fast: without full buy-in from doctors, nurses, and administrators, virtual wards fall apart.
“There’s just this complete lack of understanding of what a hospital at home service…can deliver.” – Key Informant
Without clinical confidence and clarity, referrals don’t happen, escalations stall, and patients fall through the cracks. Many providers still see HaH as a mysterious tech add-on, not as a core part of patient care.
This misunderstanding breeds confusion, and confusion in healthcare can be dangerous.
Personalized Care or Patchy Support?
On paper, HaH offers holistic, patient-centered care. Imagine a frail older adult recovering from pneumonia at home, supported by a multidisciplinary team that knows their living conditions and can tailor treatment accordingly.
But in practice? The wrong setup can derail it. If a patient doesn’t have internet, lives far from the care hub, or struggles with self-management, they may not get what they need.
“Lots of patients could be treated at home—but they don’t have an appropriate home environment.” – Key Informant
Worse, digital exclusion and rural access issues may increase health inequalities, not reduce them.
A Workforce Reimagined—But Not Yet Ready
HaH doesn’t just repackage hospital care. It reshapes who delivers it. Teams are flatter. Advanced nurse practitioners and pharmacists take the lead. The ethos: empower every team member to act at the top of their license.
But are systems and training keeping up?
“You’ve got to make sure that you’re safe—as well as your patient.” – Key Informant
Care in the home demands different skills, from working solo to navigating unfamiliar environments. Many staff lack the training or support to make this leap. Without investing in this new model of care, burnout and attrition may follow.
Communication: The Silent Risk
One theme echoed across interviews: communication—or lack of it.
In hospitals, care is centralized. Everyone’s (mostly) on the same page. At home? HaH teams must sync with primary care, social services, family caregivers, and more.
“In community, you have all these different services… It’s important to have that collaborative approach.” – Key Informant
But siloed electronic records and poorly integrated systems mean important updates fall through the cracks. Duplication, delays, and even unsafe care can result.
A fix? Shared digital systems. But many participants labeled this a “too hard to do” problem—another sobering red flag.
The Money Problem: Hidden Costs and Vanishing Budgets
Treating people at home sounds like a cost-saver. But HaH isn’t cheap. It needs specialized staff, transportation, digital devices, home visits, and more. Nearly every participant named continued funding as a weak link in the chain.
“It’s funding everything below… your equipment, your workforce.” – Key Informant
There’s also a hidden cost for patients—like paying for prescriptions that would’ve been free in hospital. For lower-income patients, this isn’t just inconvenient. It’s a barrier to care.
What’s Next for Virtual Wards?
This study is the first to create a dark logic model—a structured look at how well-meaning innovations could go sideways. It gives public health leaders and policymakers a way to plan smarter, ask harder questions, and prioritize future research.
Key takeaways:
- Buy-in from frontline clinicians is essential.
- Communication systems must be seamless and safe.
- Workforce redesign is promising—but requires investment.
- Equity risks must be addressed proactively.
These models don’t offer all the answers—but they give us the right questions to ask.
Join the Conversation
- If your community had a Hospital at Home program, what would it take to make it truly work for everyone?
- Do you think virtual wards can really reduce health inequalities—or might they unintentionally widen the gap?
- How would you design better communication between home-based teams and traditional health services?
Don’t Let Science Pass You By
⚠️ Public health breakthroughs and threats are happening fast.
Missing one update could mean missing the chance to act, advocate, or lead. Stay sharp, stay informed—with our weekly science brief, trusted by changemakers.✅ Subscribe now—it’s free and essential.
📣 Share this blog to grow the circle of informed action.



