Bringing Addiction Treatment to Those in Need
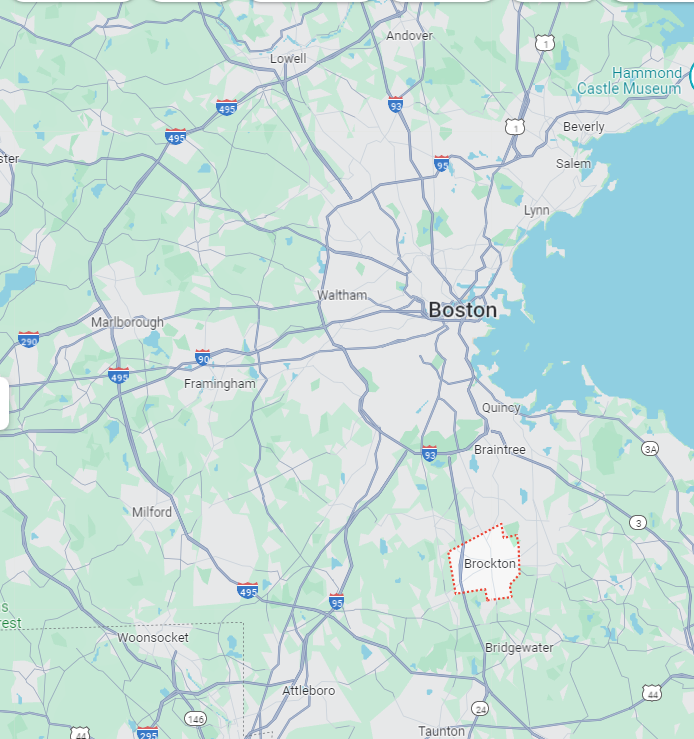
Opioid overdose deaths have been steadily increasing in the U.S., and the numbers are particularly alarming among Black, Latine, and Indigenous communities, as well as among people experiencing homelessness. While medications for opioid use disorder (MOUD) can be lifesaving, only a small fraction of eligible individuals actually receive them. To address this gap, a new initiative in Brockton, Massachusetts, is bringing hope and treatment directly to those who need it most.
The Birth of a Mobile MOUD Unit
In September 2021, the Brockton Neighborhood Health Center (BNHC) launched a mobile MOUD unit with support from the HEALing Communities Study coalition. The goal was simple yet ambitious: to improve access to addiction treatment in Brockton, a racially diverse city with a high rate of opioid overdose deaths, especially among Black residents.
The mobile unit, known as Community Care-in-Reach®, offers low-threshold buprenorphine (an effective MOUD), harm reduction supplies, and preventive care. This approach was designed to reach those who might not access traditional brick-and-mortar clinics due to various barriers, including stigma, transportation issues, or mistrust of the healthcare system.
Overcoming Challenges to Serve the Community
Setting up and running the mobile unit was no small feat. The team faced numerous challenges, from securing local buy-in and navigating complex licensure processes to maintaining operations during the COVID-19 pandemic and planning for long-term sustainability. Despite these hurdles, the mobile unit has made significant strides in just two years.
Since its launch, the mobile team has cared for 297 unique patients over 1,286 visits. More than one-third of these patients received buprenorphine prescriptions, a critical step in treating opioid use disorder. Notably, the patients seen by the mobile unit were more representative of marginalized racial and ethnic groups and people experiencing homelessness compared to those seen at BNHC’s stationary clinics.
A New Model of Equitable Care
One of the key elements of the mobile unit’s success is its ability to provide a variety of services beyond MOUD. This includes wound care, syringe and safer smoking supplies, naloxone (a medication that can reverse opioid overdoses), and other basic medical care. By offering these services in an on-demand, nonjudgmental setting, the mobile unit has been able to engage individuals who might otherwise avoid seeking help.
For many patients, the mobile unit represents a lifeline. It brings essential services to convenient locations, such as areas where overdoses frequently occur, making it easier for individuals to access care without the need for transportation or navigating a complex healthcare system.
Why This Matters
The mobile MOUD unit in Brockton is more than just a medical service; it’s a beacon of hope for communities that have been historically underserved and disproportionately affected by the opioid crisis. By providing equitable access to addiction treatment and harm reduction services, the mobile unit is helping to address systemic disadvantages and save lives.
For public health practitioners, this initiative serves as a powerful example of how innovative, community-focused approaches can make a tangible difference in the fight against opioid addiction. It highlights the importance of flexibility, cultural competence, and nonjudgmental care in reaching and supporting marginalized populations.
Engaging the Community
The success of the mobile MOUD unit is also a testament to the power of community collaboration. The HEALing Communities Study coalition brought together a diverse group of stakeholders, including local health leaders, community organizations, and residents, to design and support the initiative. This collective effort has been crucial in overcoming challenges and ensuring the program’s sustainability.
Looking Ahead
While the mobile unit has already made significant progress, there is still much work to be done. The team continues to seek funding and advocate for supportive policies that will allow the program to expand and thrive. Key areas of focus include securing grants, maximizing billable encounters, and ensuring state-level policies support mobile and telehealth services.
As the opioid crisis continues to evolve, initiatives like Brockton’s mobile MOUD unit offer a blueprint for how to effectively address addiction in marginalized communities. By prioritizing equity, accessibility, and community engagement, we can make strides toward a future where everyone has the opportunity to receive the care they need.
Be Part of the Change – Get Weekly Updates!
Stay informed and connected. Subscribe for free and share this blog to make a difference in public health with others.