
Empowering Health Equity: Lessons from the CDC’s CORE Initiative
Health equity is more than just a buzzword—it’s a mission to ensure that everyone has the same opportunities for a healthy life, regardless of their background. In 2021, the Centers for Disease Control and Prevention (CDC) launched the CORE initiative, embedding health equity as a foundational component of their work. This initiative has led to significant insights into how state and local health departments can advance health equity. A recent study published in the Journal of Public Health Management and Practice explores the CDC’s Health Equity Science (HES) framework and its implementation at various health departments. Let’s dive into the key findings and why they matter.
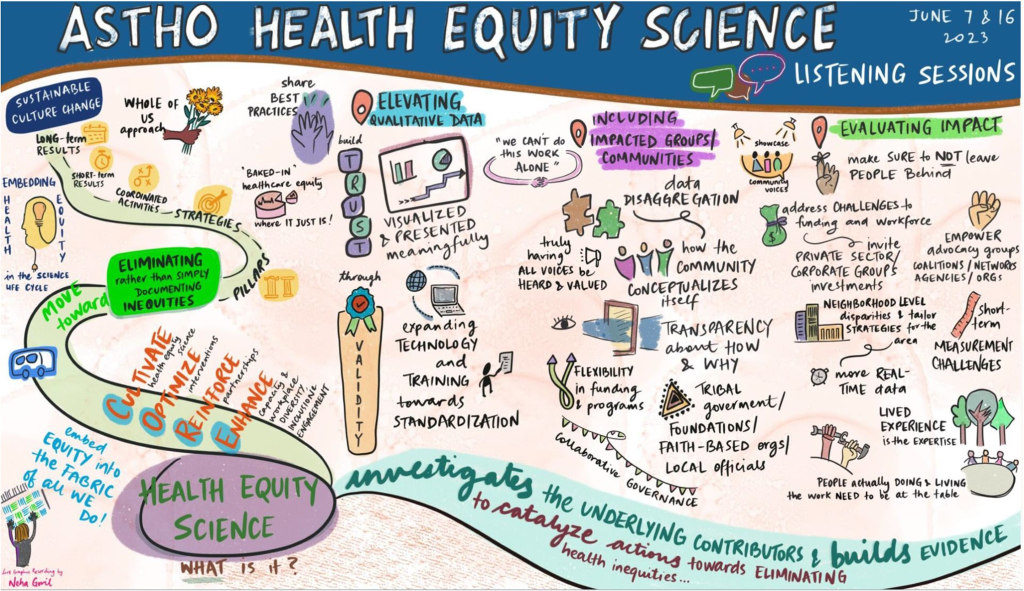
The CORE Initiative and HES Framework
The CDC’s CORE initiative stands for Cultivating Comprehensive Health Equity Science. It aims to move beyond merely documenting health inequities to investigating their root causes and promoting actionable solutions. The HES framework guides this effort by focusing on several key principles:
- Enhancing the evidence base for health equity.
- Addressing interdisciplinary public health practice and data needs.
- Recognizing the value of qualitative data.
- Evaluating health equity programs and policies.
- Including impacted communities in every step of health equity efforts.
These principles are designed to create a robust, actionable approach to tackling health disparities.
Key Findings from the Study
The study involved consultations and discussions with state and local health departments and community partners across five states. Here are the five major themes that emerged:
- Enhancing the Health Equity Evidence Base: There’s a need for more scalable, replicable, and timely health equity data. Health departments emphasized the importance of creating a comprehensive library of evidence-based interventions and improving data systems to capture real-time information.
- Interdisciplinary Public Health Practice and Data Needs: Effective health equity work requires integrating public health with other disciplines like transportation, infrastructure, and housing. Health departments called for standardized health equity terminology and better data standards to support this integrative approach.
- The Value of Qualitative Data: Quantitative data alone can’t capture the full picture of health inequities. Elevating qualitative data—stories and experiences from the community—provides critical context and deeper understanding.
- Evaluating Health Equity Programs and Policies: Robust evaluation is essential for improving health equity interventions. Health departments need support and training in evaluation methods to assess the impact of their programs effectively.
- Including Impacted Communities: True health equity efforts must involve those directly affected by health disparities. This means engaging community members in the planning, implementation, and evaluation of health equity initiatives.
Why This Matters
Health inequities affect everyone. They lead to poorer health outcomes and higher healthcare costs, and they reflect broader societal injustices. By addressing these inequities, we can create healthier communities where everyone has the opportunity to thrive.
The HES framework and the insights from this study provide a roadmap for health departments to strengthen their health equity efforts. For instance, enhancing the evidence base helps public health officials make more informed decisions. Including community voices ensures that interventions are culturally appropriate and more likely to succeed.
Practical Implications
For health departments looking to implement these findings, here are a few practical steps:
- Invest in Data Systems: Improve data collection and sharing practices to ensure timely and comprehensive health equity data.
- Foster Interdisciplinary Collaboration: Work with other sectors to address the broader social determinants of health.
- Elevate Community Voices: Engage community members in meaningful ways and value their qualitative input.
- Prioritize Evaluation: Allocate resources and training to evaluate the impact of health equity programs effectively.
- Build Trust: Develop long-term strategies for community engagement to build trust and sustain partnerships.
What do you think?
Discussion Questions
- How can your local community get involved in health equity initiatives?
- What are some challenges you see in integrating health equity into public health practice?
Conclusion
The CDC’s CORE initiative and the HES framework offer powerful tools for advancing health equity. By understanding and implementing the insights from this study, health departments can make significant strides in reducing health disparities. It’s not just about better health data or more effective programs; it’s about creating a fairer, healthier world for everyone.
Stay Ahead in Public Health – Get Your Weekly Update!
Want to be a leader in health? “This Week in Public Health” gives you key updates every week. Our newsletter shares news on the latest breakthroughs and projects, helping you stay informed. Subscribe for free and help shape the future of public health today!



