How This Study Could Help Millions Manage Brain Fog
“Sorry, I’m just feeling foggy today.”
We’ve all said it. Maybe after a bad night’s sleep or a stressful week. But what if that fog didn’t lift after a nap or a weekend off? What if it lingered for months—or years?
According to recent research, brain fog is far more than a fleeting annoyance. It affects 28.2% of adults and has emerged as a serious global public health concern, particularly in the wake of long COVID and other chronic illnesses. And yet, we still don’t fully understand what brain fog is—or how to prevent or treat it.
Let’s unpack why this everyday experience is anything but ordinary—and what needs to happen next.
Brain Fog: More Than Just a “Fuzzy Feeling”
Imagine waking up and feeling like your brain is running through molasses. Your thoughts come slowly, concentration slips, and even simple conversations feel like puzzles. Now imagine living like that, not for a day, but for months.
That’s what brain fog feels like for millions. It’s a form of cognitive dysfunction that slows thinking, muddies memory, and dulls mental sharpness. It commonly shows up in people with long COVID, cancer, kidney disease, HIV, pregnancy, and mental health conditions. But here’s the kicker: even people without chronic illness experience it—especially after stress, infection, or poor sleep.
For some, it’s a bump in the road. For others, it’s a full-on derailment of daily life, career, and relationships.
A Public Health Problem Hiding in Plain Sight
So why are we just now paying serious attention to brain fog?
Partly because the COVID-19 pandemic turned a spotlight on it. Up to 62% of long COVID survivors report cognitive issues—often lasting well beyond recovery. That means millions globally are living with long-term brain fog, adding to healthcare burdens and lost productivity.
But even before the pandemic, many cancer survivors, kidney patients, and people with autoimmune diseases were quietly navigating these same symptoms. Thanks to medical advances, more people are surviving serious illnesses—but they’re also left grappling with long-term side effects like brain fog.
It’s not just about memory lapses. Brain fog can prevent people from returning to work, caring for family, or even recognizing themselves. It’s tied to depression, anxiety, and declining quality of life, making it a silent multiplier of mental health challenges.
The Big Questions Science Still Can’t Answer
Here’s where the fog thickens. Researchers agree: we still don’t really know what brain fog is.
Some people report severe mental cloudiness, but cognitive tests show they’re fine. Others score poorly on tests but say they feel okay. That disconnect raises tough questions:
- Is brain fog the same across different illnesses?
- Can we prevent it with early interventions?
- Why do some treatments work for some people but not others?
We don’t even have a universally accepted definition. A new Brain Fog Scale helps capture symptoms more consistently, but more research is needed—especially with input from people living with brain fog, not just scientists.
Small Wins—and Big Gaps—in Treatment
There’s some hope. Interventions like exercise, better nutrition, cognitive rehab, and mental health support show promise—especially for people undergoing planned treatments like chemotherapy. But these approaches are rarely used in routine care, and their long-term effects aren’t well understood.
There’s no one-size-fits-all solution. And for the broader population, evidence-based prevention strategies are almost nonexistent.
Why This Matters Now
Brain fog isn’t going away. If anything, it’s becoming more common. As we live longer and recover from serious illnesses more often, cognitive side effects will be a growing part of the public health landscape.
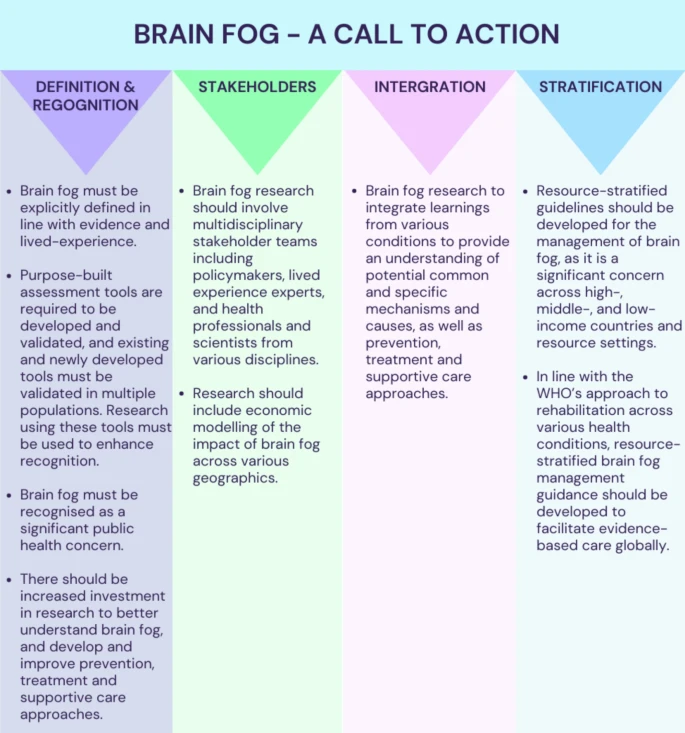
That’s why researchers behind this study issued a call to action:
- Fund more research to define, measure, and understand brain fog.
- Develop targeted treatments that work across diverse populations.
- Include lived experience voices in designing solutions.
- Recognize brain fog as a legitimate, chronic condition in clinical care.
What’s Next for Public Health?
If you work in public health, mental health, or clinical care, brain fog deserves your attention. It’s affecting your patients, your coworkers, and maybe even you. This isn’t just about memory—it’s about dignity, functionality, and quality of life.
We need to bring brain fog out of the shadows and into our policies, funding decisions, and everyday care.
Join the Conversation
What’s your experience with brain fog?
Have you seen it impact your community or workplace?
What do you think public health should do next?
Let’s keep the conversation going. Share your story or insights in the comments—or pass this along to someone who needs to see it.