Understanding Overdose Spikes
Imagine you’re a public health official in Massachusetts. After weeks of routine overdose data reporting, a sudden spike in deaths hits your desk: an alarming five extra fatalities in just one day. What caused this? A bad batch of fentanyl? A sudden lapse in services? These are not just hypothetical questions. They highlight the challenges communities face when overdose deaths surge unpredictably, often without warning.
A new study offers fresh insights into these overdose “spikes,” using advanced algorithms to track short-term surges in deaths. Unlike traditional approaches that focus on long-term trends, this study digs deep into daily variations to uncover patterns that could save lives.
Why Focus on Spikes?
Over the past two decades, drug overdose deaths in the U.S. have skyrocketed, claiming hundreds of thousands of lives. Public health strategies often rely on long-term data to guide interventions and allocate resources, but this big-picture approach can miss critical short-term events like overdose spikes. These sudden surges, though fleeting, account for a significant share of deaths. Understanding them better could mean the difference between a rapid, targeted response and a missed opportunity to save lives.
The Massachusetts study analyzed over 16,000 overdose deaths between 2017 and 2023. By employing a sophisticated spike detection algorithm, researchers identified days when fatalities rose dramatically above expected levels. Their findings could transform how we monitor and respond to overdoses, offering a roadmap for more nimble public health responses.
Key Findings: Short-Term Fluctuations with Big Impacts
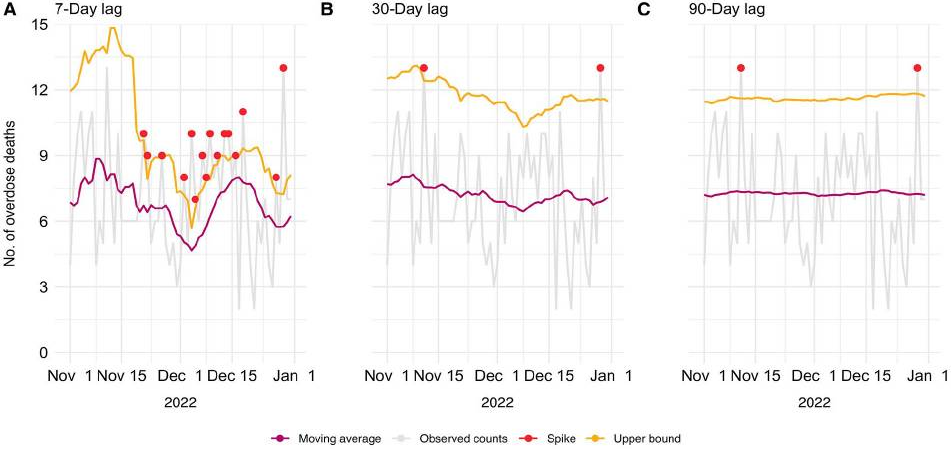
The study revealed that spikes are not rare anomalies—they are a persistent part of the overdose landscape. Depending on the detection method, between 5.8% and 20.6% of days each year were classified as spike days. These accounted for as much as 31.6% of all overdose deaths annually. On average, three to six additional deaths occurred on spike days compared to non-spike days.
Interestingly, the method used to define a spike significantly affected the results. Shorter timeframes (like a 7-day moving average) captured more frequent, smaller spikes, while longer timeframes (like a 90-day moving average) identified fewer, but larger, surges. This flexibility is a double-edged sword: it allows customization for local needs but also highlights the lack of a universal definition for what constitutes a spike.
Why Do Spikes Happen?
Understanding why spikes occur is crucial for prevention. The study suggests several potential triggers, including changes in the drug supply, such as batches laced with fentanyl, or disruptions in access to addiction treatment or mental health services. External factors like economic downturns or sudden policy changes might also contribute.
To illustrate, consider a hypothetical scenario: a new, potent synthetic opioid enters the illicit market in Boston. Within days, overdose deaths double, overwhelming emergency responders. Without a system to detect and respond to these spikes, lives that could have been saved with naloxone distribution or public alerts are lost.
Practical Applications: A Call to Action
The study’s findings are more than academic—they offer actionable insights for public health practitioners and policymakers:
- Enhanced Surveillance Systems: Real-time monitoring systems could detect overdose spikes faster, allowing for rapid responses such as targeted naloxone distribution or public warnings.
- Tailored Interventions: Communities could adapt spike definitions to local conditions, focusing resources where they are needed most.
- Cross-Sector Collaboration: Public health agencies, law enforcement, and harm reduction groups must work together to identify and respond to spikes. For example, Rhode Island has used nonfatal overdose data to predict and respond to spikes, reducing opioid deaths by 8.3% from 2016 to 2019.
What’s Next?
While this study provides a strong foundation, it also raises important questions. For instance, how do specific drugs contribute to spikes? Could real-time data from emergency medical services or community organizations improve detection? And how can we prevent alert fatigue among responders, ensuring that every spike warning leads to meaningful action?
Future research should also explore regional differences. While this study focused on Massachusetts, overdose trends vary widely by location. What works in an urban setting may not apply to rural communities, where resources are scarcer, and distances greater.
Join the Conversation
This study underscores the urgency of addressing overdose spikes with precision and speed. It’s a call to innovate, collaborate, and act—because lives depend on it.
What strategies have you seen work in responding to sudden health crises in your community? How can we balance the need for rapid alerts with the risk of desensitization? And what role do you think community members should play in designing solutions?
Be Part of the Change – Get Weekly Updates!
Stay informed and connected. Subscribe for free and share this blog to make a difference in public health with others. If you liked this blog, please share it! Your referrals help This Week in Public Health reach new readers.



