
The Power and Challenges of America’s New Suicide Prevention Number: Georgia’s Experience
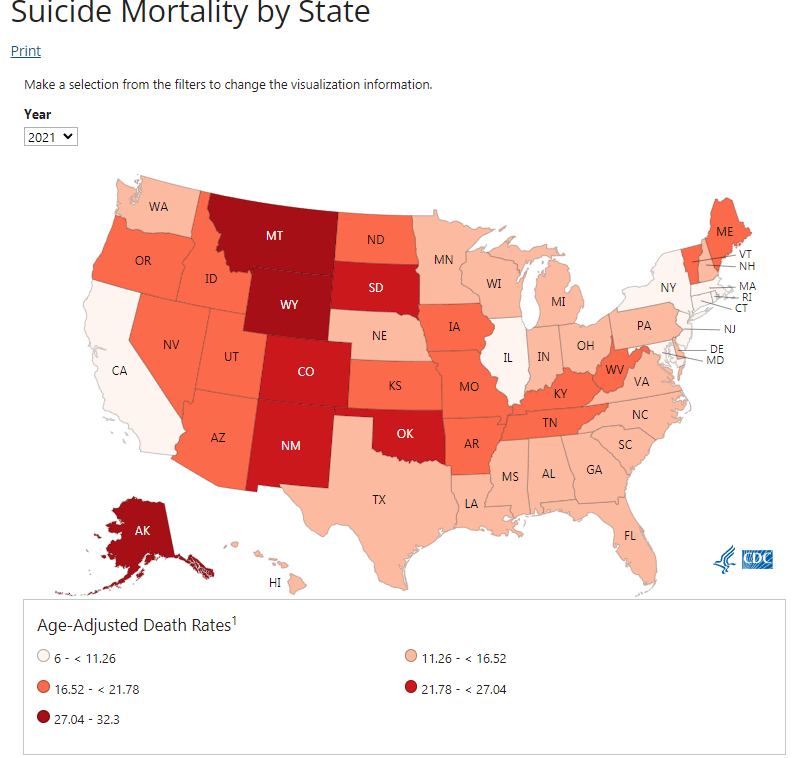
In recent years, suicide has emerged as a critical public health issue in the United States. The surge in suicide rates, compounded by the devastating effects of the COVID-19 pandemic and the ongoing opioid epidemic, has pushed mental health to the forefront of national concern.
This growing urgency has catalyzed significant federal responses, including the establishment of 988 as the new, universal telephone number dedicated to suicide prevention. But how effective is this new tool in the battle against mental health crises?
Understanding the Scope of the Problem
The statistics paint a grim picture: from 2000 to 2020, suicide rates in the U.S. have increased by a startling 30%. Moreover, in the shadow of the pandemic, over 12 million American adults contemplated suicide in a single year. The need for effective crisis intervention has never been more apparent. Emergency departments, often the first line of defense, are overwhelmed and underprepared to handle mental health crises, resulting in long wait times and inadequate care.
The Birth of 988
Against this backdrop, the National Suicide Hotline Designation Act of 2020 was signed, giving rise to 988 — a number easy to remember, aiming to make mental health support as accessible as emergency medical services. This initiative seeks to provide immediate, 24/7 assistance to anyone in a mental health crisis or contemplating suicide, thus decriminalizing mental health issues and offering a direct line to help without the need for law enforcement involvement.
Evaluating 988’s Impact in Georgia
Georgia serves as a critical case study for understanding the effectiveness of 988. The state’s pre-existing robust infrastructure for handling mental health crises gave it a distinct advantage when transitioning to the federally mandated 988 system. This foundation not only facilitated a smoother integration but also set the stage for a comprehensive understanding of how existing systems can enhance new initiatives.
Starting from Strength
Prior to the introduction of 988, Georgia had already developed a comprehensive network for mental health support through its statewide suicide hotline. This system was not merely about answering calls; it included extensive training for hotline staff, a well-coordinated network of support services, and a solid technological infrastructure. This pre-existing framework meant that Georgia was not starting from scratch but rather enhancing and expanding its capabilities with the integration of 988.
Early Outcomes and Insights
The introduction of 988 in Georgia was met with significant uptake, reflecting both the ongoing need for mental health services and the public’s trust in the system’s efficacy. In the first six months post-launch, the 988 Lifeline’s more than 2.1 million contacts (calls, chats, and texts) underscored a critical demand for accessible mental health services. This high volume of contacts suggests that the hotline is reaching a broader audience than previously engaged by traditional mental health services, potentially tapping into a demographic that had not accessed help due to stigma, lack of information, or previous inaccessibility of services.
System Enhancements and User Experience
One of the key successes observed in Georgia was the immediate availability and responsiveness of the 988 service. Unlike traditional emergency services that often struggle with high call volumes and long wait times, 988 was designed to be more immediate and direct. Georgia’s experience highlights how a well-oiled infrastructure can lead to efficient service delivery. Callers typically experienced short wait times, and many issues were resolved directly over the phone, reducing the need for further emergency interventions.
Challenges and Opportunities
However, the transition to 988 is fraught with complexities and challenges. While initial federal funding provided a significant boost to kick off the initiative, the sustainability and expansion of 988 services hinge critically on state and local funding. This dependence on varied legislative environments across the country has led to a patchwork of support, where the robustness of services can vary dramatically from one state to another.
Funding Inconsistencies and Legislative Hurdles
Unfortunately, legislative support for these essential services has not been uniformly enthusiastic or effective across all states. Only a few states have successfully passed legislation that provides sustainable funding mechanisms for their local 988 centers. This creates a significant disparity in the quality and availability of services offered through 988, potentially leading to a postcode lottery where the effectiveness of suicide prevention efforts is heavily dependent on one’s geographic location.
The inconsistency in legislative support can be attributed to a variety of factors, including political priorities, economic constraints, and differing levels of awareness about mental health issues. In some regions, mental health still struggles to be recognized as a priority equal to physical health, affecting the allocation of state and local budgets. Moreover, some states face budgetary constraints that make it challenging to allocate funds for new initiatives, regardless of their potential impact on public health.
Impact of Funding Gaps
These funding gaps have direct consequences on the operational capabilities of 988 services. In states where legislative support has lagged, 988 centers may struggle with insufficient staffing, limited training resources, and outdated technological infrastructure. This can lead to longer wait times, reduced effectiveness in crisis intervention, and a diminished ability to follow up with individuals who reach out for help.
The Need for a Uniform Approach
The stark variation in funding and support underscores the need for a more uniform approach to the implementation of 988 across the United States. Ensuring that every individual in crisis has access to high-quality support should not be contingent on state borders. Federal incentives or mandates may be necessary to harmonize the level of services provided nationwide, ensuring that every call, text, or chat to 988 receives the attention and care it deserves.
Policy Recommendations and Future Directions
For 988 to truly make a difference, the authors argue that the system must be part of a comprehensive mental health crisis care system that does not stop with immediate crisis intervention. Continuous care and support, integrated with community services and backed by adequate funding, are essential for the long-term effectiveness of 988. States, including Georgia, must invest in training more mental health professionals and ensuring that these services are accessible to all, particularly in rural and underserved areas.
Conclusion: A Call to Strengthen Our Mental Health Infrastructure
The implementation of 988 is a significant step forward in addressing the mental health crisis in America. However, it’s just the beginning. The journey to better mental health care is long and complex, but with continued effort and investment, 988 can be a cornerstone of a healthier, more supportive society.
Lead the Way in Public Health – Get Your Weekly Insight!
Ready to lead the charge in health advocacy and research? ‘This Week in Public Health’ delivers essential weekly updates, keeping you informed and ahead in the dynamic field of public health. With insights on the latest breakthroughs and initiatives, our newsletter is your gateway to being a proactive leader. Subscribe for free and start shaping the future of public health today!
About the Author
Jon Scaccia, with a Ph.D. in clinical-community psychology and a research fellowship at the US Department of Health and Human Services with expertise in public health systems and quality programs. He specializes in implementing innovative, data-informed strategies to enhance community health and development. Jon helped develop the R=MC² readiness model, which aids organizations in effectively navigating change.



