Nurse Turnover: Bullying’s Hidden Cost
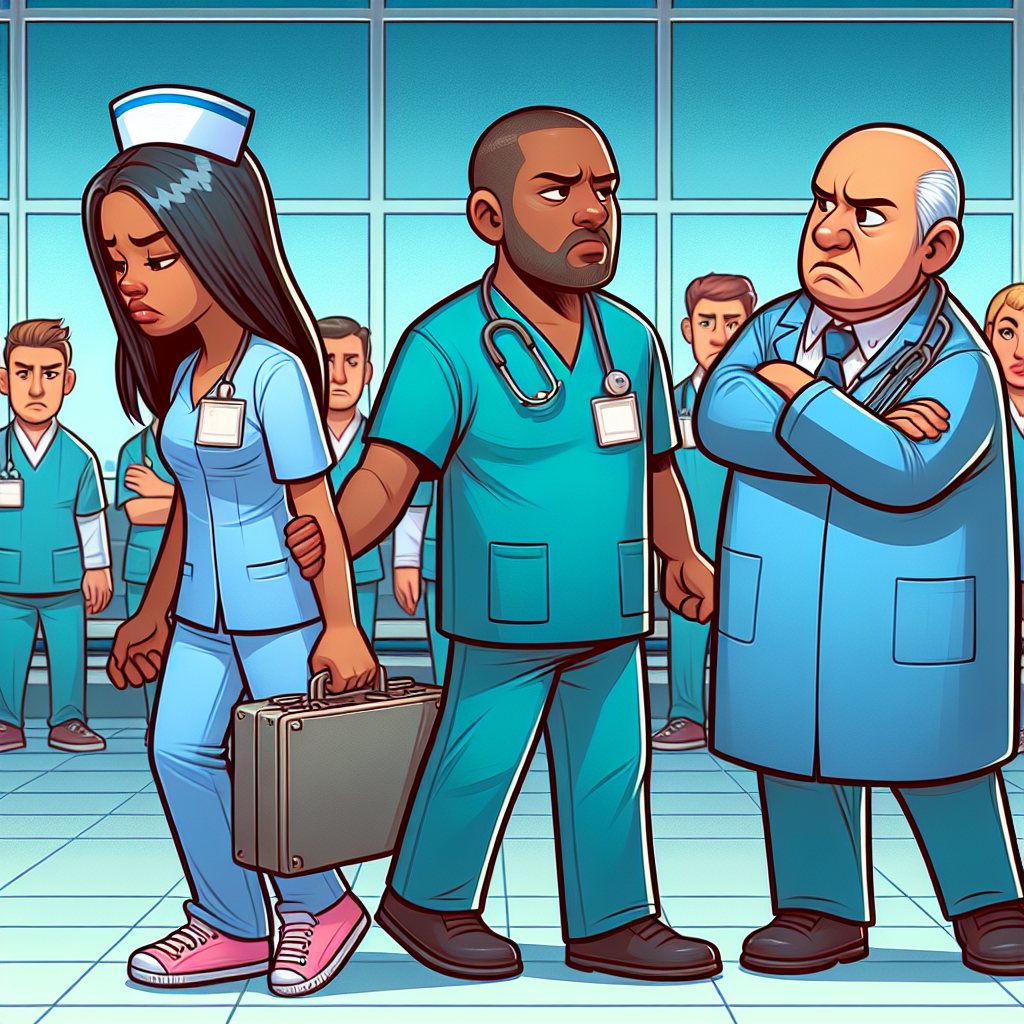
At a bustling hospital in Ghana’s Upper West Region, a young nurse stands at a crossroads, facing a challenging decision. The relentless whispers of discontent echo through the wards, surfacing as grim thoughts swirling in her mind: ‘Should I stay, or should I quit?’ This inner turmoil reflects a growing crisis in healthcare, one that extends beyond physical fatigue to the psychological toll exacted by workplace bullying among nurses.
The Pressing Issue: Workplace Bullying in Nursing
Workplace bullying (WPB) is a grave concern that transcends borders. Defined as repeated, offensive behaviors intended to harm, this phenomenon is particularly acute in nursing, a profession under immense pressure due to global staff shortages, an aging population, and an increasing burden of non-communicable diseases. A recent study highlights that WPB is not only detrimental to nurses’ mental health but also a significant predictor of their intention to leave the profession—often a precursor to actual turnover.
Study Insights: Connecting the Dots
The study conducted on 323 nurses in Ghana revealed startling statistics: 64.4% of the nurses had contemplated quitting, while 52.1% exhibited signs of depression. Further analysis demonstrated that bullying directly correlated with both the intention to quit and depression, posing a dual threat to the sustainability of healthcare services.
What This Means in Practice
- For Local Health Departments: Implement anti-bullying policies and foster a supportive workplace culture to retain staff.
- NGOs and Community Programs: Provide mental health support services for healthcare workers to mitigate the impact of bullying.
- Policy Makers: Advocate for resources and regulatory frameworks to address WPB and nurse retention proactively.
Translating Complexity into Action
The methods involved deploying a structured questionnaire among two primary groups of nurses—Registered General Nurses and Enrolled Nurses—capturing data on bullying incidents, depression levels, and intentions to quit. The results, indicative of a strong positive correlation, illuminate the cascading effects of WPB, from increased job dissatisfaction to the very real prospect of compromised patient care.
What’s Next & Barriers
Future Pathways
Acknowledging WPB as both a psychological hazard and a factor in workforce turnover, healthcare leaders must integrate WPB indicators into their strategic planning. Potential policy adoption includes zero-tolerance bullying policies, routine mental health evaluations, and creating safe channels for reporting bullying incidents.
Barriers & Constraints
The impediments to addressing WPB are multifaceted. Financial constraints, ingrained organizational cultures, and limited awareness of mental health advocacy pose significant hurdles. Moreover, the social stigma surrounding mental health and bullying must be dismantled to pave the way for substantive reform.
Reflective Dialogue: A Call to Action
This research calls on all stakeholders to reassess the current organizational climate. How might your agency adapt these findings locally? Furthermore, addressing resource and policy constraints could improve nurse retention and well-being. What resource limitations might hinder these applications? Finally, reconsider your assumptions about WPB—does this data challenge longstanding beliefs in your professional environment?
By tackling WPB head-on, we cultivate not just a healthier working environment but also nurture the resilience of the healthcare workforce our communities desperately rely on.
For further reading, explore the full study at PLOS ONE.



