
Fentanyl Overdoses Are Falling — But Not for Everyone
A public health story about progress, gaps, and what emergency departments can do next
At 2:30 a.m., an emergency department clinician administers naloxone to a young adult found unconscious in a parking lot. The patient survives. By morning, the ED is full again — overdoses, injuries, psychiatric crises, all colliding in the same space. For years, fentanyl has been the common thread running through these encounters. Now, new national data suggest something has shifted.
According to a recent CDC Morbidity and Mortality Weekly Report, emergency department visits for suspected fentanyl-involved nonfatal overdoses rose steadily from late 2020 through mid-2023, then began to decline through early 2024. On the surface, this looks like welcome news. But beneath that trend line lies a more complicated — and more urgent — story
Why Nonfatal Overdoses Matter More Than We Think
Public attention often centers on overdose deaths. But nonfatal overdoses are one of the strongest predictors of future fatal overdose. Each ED visit is both a warning sign and a rare opportunity for intervention.
This study used near-real-time emergency department data from the CDC’s National Syndromic Surveillance Program, covering about 80 percent of U.S. EDs. Researchers analyzed quarterly rates of fentanyl-involved nonfatal overdose visits from October 2020 through March 2024, broken down by age, sex, and race and ethnicity.
The approach matters: instead of waiting months or years for finalized mortality data, syndromic surveillance shows what is happening now.
What the Data Show — In Plain Language
The Big Picture
- From late 2020 to mid-2023, ED visits for fentanyl nonfatal overdoses rose sharply, increasing nearly 9 percent per quarter.
- After peaking in mid-2023, rates declined about 11 percent per quarter through early 2024.
- Even with the decline, the rate in early 2024 was still double what it was in 2020.
Key insight: Decline does not mean resolution.
Who Is Most Affected?
Age
- Adults aged 25–34 had the highest overdose visit rates.
- Younger adults (15–24) saw increases later than other groups but also experienced recent declines.
- Adults over 55 showed steady increases until mid-2023, followed by modest declines.
Sex
- Males consistently had much higher rates than females.
- Both groups followed the same rise-and-fall pattern, though declines among females were less pronounced.
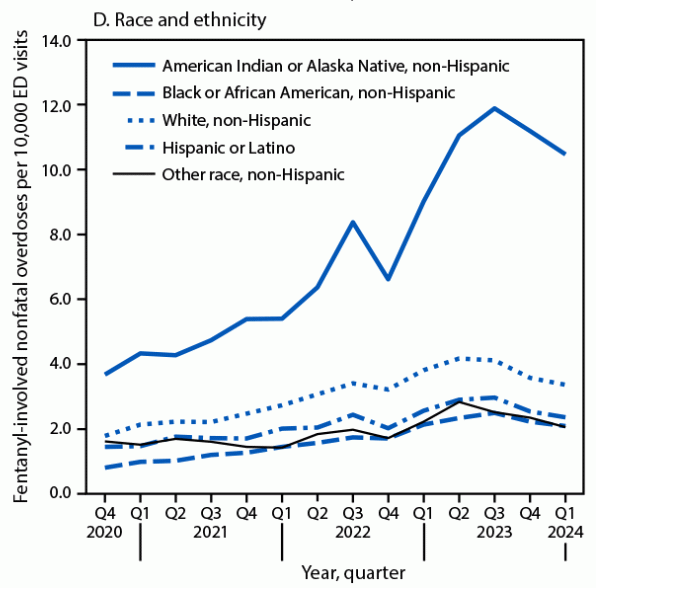
Race and Ethnicity
This is where the data are most stark.
- American Indian and Alaska Native (AI/AN) communities experienced:
- The highest overdose rates by far.
- The largest increases over time.
- No statistically significant decline after mid-2023.
Rates among Black, White, and Hispanic populations did decline — but unevenly.
Why Emergency Departments Matter So Much
Emergency departments are often the only point of care for people at highest risk of overdose. The study reinforces what many practitioners already know: EDs are not just treatment sites — they are prevention hubs. Evidence-based ED actions include:
- Initiating buprenorphine for opioid use disorder on the spot.
- Distributing naloxone to patients and families.
- Linking patients to ongoing care, including peer recovery support.
- Screening for mental health conditions, which frequently co-occur with overdose risk.
“A nonfatal overdose is not the end of a crisis. It is the clearest signal that intervention must happen now.”
What This Means in Practice
For Local Health Departments
- Use ED overdose data to target outreach geographically and demographically.
- Partner with hospitals serving AI/AN communities to co-design prevention strategies.
- Align overdose prevention with behavioral health and housing initiatives.
For Emergency Departments
- Make ED-initiated medication for opioid use disorder the default, not the exception.
- Build warm handoffs to community treatment and recovery services.
- Stock naloxone and normalize discharge with overdose prevention kits.
For Community-Based Organizations
- Focus on post-overdose engagement, not just primary prevention.
- Train peers with lived experience to work alongside ED teams.
- Address trust gaps, especially in communities with historical trauma.
Barriers and Open Challenges
Despite progress, major obstacles remain:
- Workforce shortages limit ED capacity for follow-up care.
- Inconsistent toxicology testing may undercount fentanyl involvement.
- Racial misclassification likely underestimates impacts on AI/AN populations.
- Funding silos separate overdose prevention from mental health services.
And perhaps most critically: declines may not last without sustained investment.
What’s Next?
The study raises urgent questions:
- Are declines driven by policy, supply changes, treatment access — or something else?
- Why are some communities not seeing the same benefits?
- How can ED-based interventions be scaled without burning out staff?
Monitoring trends is not enough. The next phase of overdose prevention must focus on who is still being left behind.
Conversation Starters
- How is your agency using ED overdose data right now?
- What would it take to make ED-initiated treatment routine in your community?
- Does this challenge assumptions about where the overdose crisis is “improving”?
Bottom line: Fentanyl nonfatal overdoses may be declining nationally, but the crisis remains deeply unequal. Emergency departments are one of the few places where prevention, treatment, and recovery can intersect in real time. What happens there next will shape whether this decline becomes a turning point — or just a pause.



